Potent, puzzling and (now less) toxic: How antifungal drug works
Scientists have solved a decades-old medical mystery – and in the process have found a potentially less toxic way to fight invasive fungal infections, which kill about 1.5 million people a year. The researchers say they now understand the mechanism of action of amphotericin, an antifungal drug that has been in use for more than 50 years – even though it is nearly as toxic to human cells as it is to the microbes it attacks.
A report of the new findings appears in Nature Chemical Biology.
“Invasive fungal infections are a very important unmet medical need,” said University of Illinois and Howard Hughes Medical Institute chemistry professor Martin Burke, who led the study with chemistry professor Chad Rienstra. “There are about 3 million cases per year and what’s striking is that, even in 2014, half the patients who come into the hospital with an invasive fungal infection in their blood die.”
More people are killed by invasive fungal infections than by malaria or tuberculosis, Burke said.
Amphotericin (am-foe-TEHR-ih-sin) is the most effective broad-spectrum antifungal drug available, Burke said. But its use is limited by its toxicity to human cells.
“When I was a medical student, they used to call it ‘amphoterrible’ in the clinic because it has very powerful side effects,” he said. “And so you’re stuck between having the fungus kill the patient, versus using too much amphotericin, which kills the patient.”
Scientists have long sought to make amphotericin less toxic, but have been hindered by an obvious problem: Because it is so hard to study, no one knew exactly how it worked.
“This molecule is one of the most challenging to work with because it has a very complex structure, is poorly soluble and is sensitive to light, oxygen and acid,” Burke said.
Amphotericin also interacts with membranes, which are notoriously difficult to study. Many labs, including Burke’s, have tried to figure out the three-dimensional structure of amphotericin by crystallizing it, a standard technique. So far, all attempts have failed.
So the team turned to one of the most powerful tools for studying non-crystalline samples: solid-state nuclear magnetic resonance (NMR) spectroscopy, which measures how atomic nuclei respond to changes in a magnetic field.
“NMR is a great technique for detecting signals and interpreting the structural properties of molecules in solution,” said Rienstra, who led the NMR work with graduate students Mary Clay and Tom Anderson. But few labs use it to track interactions between small molecules in membranes, he said. “We developed several new NMR experiments to study amphotericin in the presence of membranes.”
Previous studies had found evidence that amphotericin opens up ion channels in membranes, perhaps making them more leaky to charged atoms that could disrupt a cell. Most scientists assumed that this was the drug’s main mode of action.
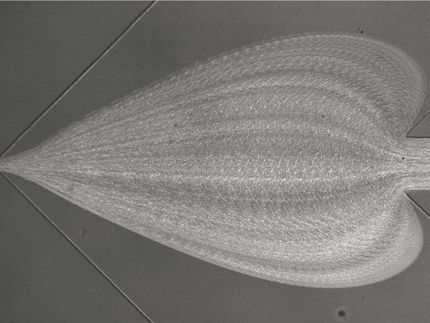
But the evidence also suggested that amphotericin interacted with sterols, such as cholesterol in animal cells and ergosterol in yeast. Rienstra and Burke focused on amphotericin’s influence on sterols, hypothesizing that this might be a key to its toxicity.
The initial NMR data supported this idea, indicating that very little of the drug – less than 5 percent – actually formed channels in membranes. Using NMR and other experimental tools, the Rienstra/Burke team found that most of the amphotericin aggregates on the exterior of membranes, extracting sterols out of membranes like a sponge. Cell death follows soon after.
“For over 50 years, the mechanism by which amphotericin kills cells has remained a mystery,” Burke said. “But we are finally seeing the fog start to clear. This new understanding allows us to focus on how to make this molecule less toxic to human cells.”
In a separate study published in the Journal of the American Chemical Society, Burke and his colleagues appear to have accomplished just that. They developed a derivative of amphotericin that, at least in cell culture, binds to ergosterol in yeast but not to human cholesterol.
“We are very excited about this discovery,” Burke said. “But a great deal of work lies ahead to see if this compound has the potential to serve as a less toxic treatment for fungal infections in human patients. At this point, we just have a very promising compound. Most importantly, thanks to the collaboration between these two labs, we now know where to look for solutions to this longstanding problem.”
Preclinical trials of the new compound have begun, the researchers said.