Antibiotic levels measurable in breath for first time
Researchers are testing a biosensor for personalized dosing of medications
A team of engineers and biotechnologists at the University of Freiburg has for the first time shown in mammals that the concentration of antibiotics in the body can be determined using breath samples. The breath measurements also corresponded to the antibiotic concentrations in the blood. The team’s biosensor – a multiplex chip that allows simultaneous measurement of several specimens and test substances – will in future enable personalized dosing of medicines against infectious diseases on-site and help to minimize the development of resistant strains of bacteria.
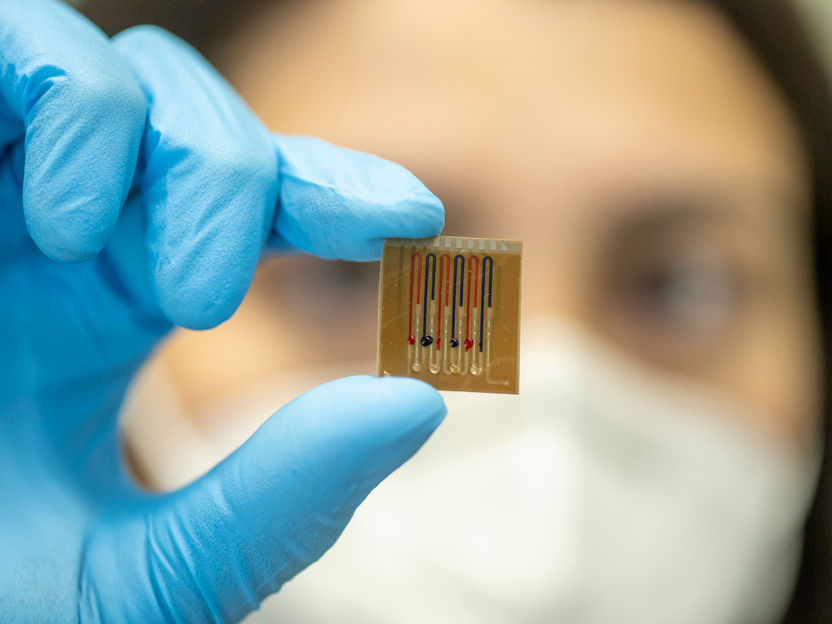
The microfluidic multiplex biosensor carries proteins attached to a polymer film that recognize the antibiotics.
Patrick Seeger, Universität Freiburg
The sensor developed by the research group headed by Dr. Can Dincer and H. Ceren Ates, FIT Freiburg Center for Interactive Materials and Bioinspired Technologies, and Prof. Dr. Wilfried Weber, Professor of Synthetic Biology and a member of the team of speakers at the Cluster of Excellence CIBSS – Centre for Integrative Biological Signalling Studies, is based on synthetic proteins that react to antibiotics and thus generate a current change. The researchers’ results are now being published in the journal Advanced Materials.
Previously researchers could only detect traces of antibiotics in the breath
The researchers tested the biosensor on the blood, plasma, urine, saliva and breath samples of pigs who had received antibiotics. They were able to show that the result achieved with biosensors in the pigs’ plasma were as accurate as the standard medical laboratory process. Previously, measurement of antibiotic levels in exhaled breath samples was not possible: “Until now researchers could only detect traces of antibiotics in the breath. With our synthetic proteins on a microfluidic chip, we can determine the smallest concentrations in the breath condensate and they correlate with the blood values,” explains Dincer.
Sensor will help to keep antibiotic level stable in severely ill
Physicians need to keep the antibiotics level within a personalized therapeutic range for patients suffering severe infections, at the risk of threats such as sepsis and organ failure or even the death of the patient. Inadequate administration of antibiotics could allow bacteria to mutate so that the medicines no longer work: they become resistant. “Rapid monitoring of antibiotic levels would be a huge advantage in hospital,” says Ates, “it might be possible to fit the method into a conventional face mask.” In another project at the University of Freiburg, Dincer is developing wearable paper sensors for the continuous measurement of biomarkers from exhaled breath. Clinical trials to validate the antibiotic biosensor by testing the system with human samples are planned.
Bacterial proteins as sensor
The microfluidic biosensor bears proteins that can recognize beta-lactam antibiotics such as penicillin, affixed to a polymer film. Antibiotic of interest in the sample and an enzyme-coupled beta-lactam are in competition to bind these bacterial proteins. This competition generates a current change – like in a battery: the more antibiotic there is present in the sample, the less enzyme product develops, which leads to a lower measurable current. The process is based on a natural receptor protein that resistant bacteria uses to detect the antibiotics that threatens them. “You could say we are beating the bacteria at their own game,” Weber says of the process developed by his group.
Original publication
Ates, H.C., Mohsenin, H., Wenzel, C., Glatz, R., Wagner, H.J., Bruch, R., Höfflin, N., Spassov, S., Streicher, L., Lozano-Zahonero, S., Flamm, B., Trittler, R., Hug, M.J., Köhn, M., Schmidt, J., Schumann, S., Urban, G.A., Weber, W., Dincer, C.; "Biosensor-enabled multiplexed on-site therapeutic drug monitoring of antibiotics"; Advanced Materials; 2021
Most read news
Original publication
Ates, H.C., Mohsenin, H., Wenzel, C., Glatz, R., Wagner, H.J., Bruch, R., Höfflin, N., Spassov, S., Streicher, L., Lozano-Zahonero, S., Flamm, B., Trittler, R., Hug, M.J., Köhn, M., Schmidt, J., Schumann, S., Urban, G.A., Weber, W., Dincer, C.; "Biosensor-enabled multiplexed on-site therapeutic drug monitoring of antibiotics"; Advanced Materials; 2021
Topics
Organizations
Other news from the department science
These products might interest you

Get the analytics and lab tech industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.