Biomarkers help predict prostate cancer progression
Researchers at Johns Hopkins have evaluated a simple, more specific blood test that identifies patients undergoing proactive surveillance for low-grade, low-stage, non-palpable prostate cancer who would eventually require treatment. These results, presented at the American Association for Cancer Research 101st Annual Meeting 2010, may be a major advance in prostate cancer risk assessment.
"Finding biomarkers that can predict future unfavorable biopsy conversion will help us to identify men with prostate cancer who may or may not need treatment," said Robert W. Veltri, Ph.D., associate professor of urology and oncology and director of the Fisher Biorepository & Biomarker Laboratory at The Brady Urological Research Institute, Johns Hopkins Hospital, Baltimore.
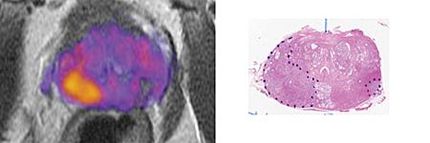
Using the novel application of the Prostate Health Index immunoassay and DNA content measurements performed by image analysis, Veltri and colleagues tested 71 patients enrolled in the Johns Hopkins Hospital Proactive Surveillance Program. The Prostate Health Index, developed by Beckman-Coulter, Inc., is a calculation involving at least three forms of free prostate-specific antigen (PSA), of which pro-PSA is one.
Thirty-nine patients developed an unfavorable biopsy, which is cancer progression defined as an increase in grade or tumor volume. The remaining patients maintained favorable biopsies. Veltri and colleagues measured serum total PSA, free PSA and pro-PSA, performed a digital rectal examination semiannually and conducted a surveillance biopsy examination each year.
Results showed that the level of Prostate Health Index was higher in men who were determined to have unfavorable biopsies, according to Veltri. Additionally, the researchers found that DNA content in biopsy tissue from the prostate gland next to the cancer area and area itself were significant predictors of a change from a favorable to an unfavorable biopsy in the Proactive Surveillance patients.
"Our findings were slightly surprising; serum pro-PSA level by itself was not able to predict unfavorable biopsy conversion in our Proactive Surveillance Program," Veltri said. "However, Prostate Health Index, which incorporates pro-PSA, free PSA and total PSA in the index, was significant for predicting unfavorable biopsy conversion."
While PSA testing may be responsible for the decreasing prostate cancer death rates occurring in the United States, Veltri said the question is raised "are we over-diagnosing and over-treating prostate cancer?"
Several studies have indicated that between 35 percent and 50 percent of men diagnosed with prostate cancer using a PSA test have cancers that would not have been detected if a PSA test had not been performed, according to Veltri. This is the case especially with low-grade, low-stage and non-palpable, small-volume prostate cancers.
"The overall objective of the Proactive Surveillance project is that baseline levels of molecular and morphologic biomarkers or other risk factors can identify men with prostate cancer who can safely forego curative intervention based upon monitoring clinical parameters and quantitative biopsy pathology," he said.
Veltri's laboratory is currently conducting an expanded study to evaluate other potential biomarkers that predict unfavorable biopsy conversion among men enrolled in the Johns Hopkins Hospital Proactive Surveillance Program.
Most read news
Topics
Organizations
Other news from the department science

Get the analytics and lab tech industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.